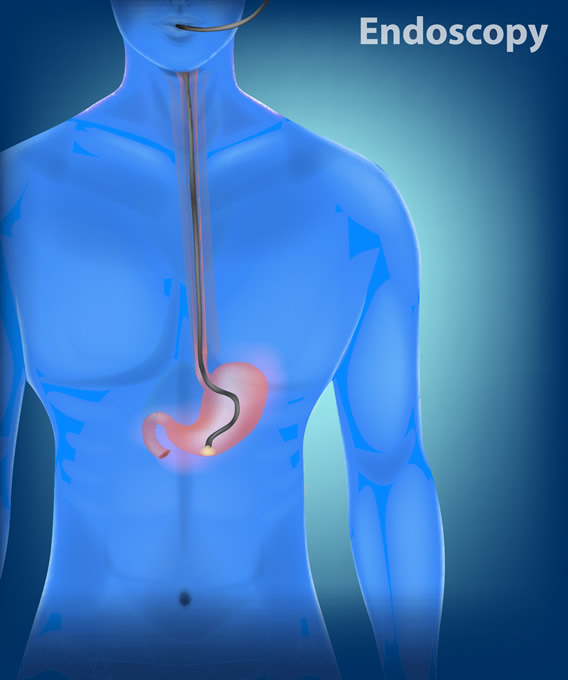
Upper Endoscopy is known as gastroscopy, EGD, or Esophagogastroduodenoscopy. It is a procedure that enables your doctor to examine the lining of the esophagus (swallowing tube), stomach and duodenum (first portion of the small intestine). A flexible, lighted tube about the thickness of your little finger is placed through your mouth and into the stomach and duodenum. The tube or “endoscope” has a lens which projects images onto a high definition video monitor. Air is pumped through the endoscope to inflate the stomach and duodenum, making it easier for your doctor to evaluate for abnormalities. Special equipment that slides through the endoscope is used, if necessary, to remove tissue samples, perform biopsies, stop bleeding, and remove abnormal growths.
There are many reasons your doctor may request an upper endoscopy. The most common include the following symptoms or diseases:
EGDs are more accurate than X-rays for detecting inflammation, ulcers or tumors of the esophagus, stomach and duodenum. It can detect cancer in very early stages and distinguish between cancerous and non-cancerous conditions.
During an EGD your doctor may remove samples of tissue or obtain a biopsy of suspicious areas which are then sent to the laboratory to be analyzed. A biopsy can be performed for many reasons and does not mean that cancer is suspected. Certain bacteria that cause ulcers or other conditions can also be diagnosed.
Upper Endoscopy requires minimal preparation.
As with all procedures it is important to advise the surgeon of all medication, vitamins and dietary supplements you are taking. Some dosages may need to be adjusted or avoided completely for a few days prior to the procedure. All allergies must be discussed with the physician or nurse as well. If you have a medical condition, such as diabetes, heart or lung disease that may require special attention during the procedure, discuss this with your physician.
When you arrive at the endoscopy center, one of our patient service coordinators will register you for your procedure. Your demographics and insurance information will be reviewed as well as your patient rights and responsibilities and privacy policy. The various consents which require your signature will be reviewed.
Patient Rights and Responsibilities
You will be asked to change into a gown. A registered nurse or an anesthesiologist will review your medical history and current medication use. Updating this information will make the procedure safe for you. Please be prepared to review your health history at this time. Bring a list of medications and drug allergies, if necessary. Please inform your physician if you have any loose dental work, or easily removed bridges.
All procedures are performed with the assistance of a board certified anesthesiologist who will monitor you before, during and after the procedure. You will be given an intravenous medication that will make most patients fall asleep. Your blood pressure, pulse rate, and oxygen saturation will be monitored before, during and after the exam.
During the procedure you may have your throat sprayed with a local anesthetic before the test begins. You will lie on your side in a comfortable position as the endoscope is gently passed through your mouth and into your esophagus, stomach and duodenum. The endoscope does not interfere with your breathing. Most patients fall asleep during the procedure. The procedure usually lasts 10-15 minutes
Following your procedure you will be monitored by a registered nurse in the recovery area until the effects of the sedatives have worn off. Most patients recover in 30-45 minutes. Your throat may be a little sore for a day or two and you may feel bloated or nauseous immediately after the procedure because of the air that is introduced into your stomach during the examination. You will be able to resume your diet and take your routine medication after you leave the endoscopy center, unless otherwise instructed.
Some results from upper GI endoscopy are available immediately after the procedure. Results of any biopsy or tissue samples take approximately 5 days to return. You will meet with your doctor after the procedure and receive preliminary results and specific instructions prior to discharge. Your escort or caretaker is expected to be available to receive these instructions as well and must sign you out of the facility (escort policy).
The sedation used during your exam impairs judgment, memory, and equilibrium. Do not drive, operate machinery, make critical decisions, drink alcoholic beverages, or do activities that require coordination or balance for 24 hours.
Potential Complications: When performed by a knowledgeable and competent physician, an Upper Endoscopy (EGD) is a very low risk procedure. Very rarely (less than 1 in 1000), bleeding or perforation (a hole or tear in the lining of the gastrointestinal tract) may occur. Other risks include a reaction to medication, irritation at the site of the injection, or complications related to other medical problems that you may already have.
Although complications after Upper Endoscopy (EGD) are rare it is important for you to recognize early signs of any possible complication. Go directly to the emergency room and contact your physician if you notice any of the following:
Please be informed that an EGD is never 100% accurate. After the procedure, if you should develop any new or recurrent gastrointestinal signs or symptoms, immediately bring it to the attention of your Physician.
There are alternatives to gastrointestinal endoscopy. Although gastrointestinal endoscopy is an extremely safe and effective means of examining the gastrointestinal tract, it is not 100 percent accurate in diagnosis. In a small percentage of cases, a failure of diagnosis or misdiagnosis may result. Other diagnostic or therapeutic procedures, such as medical treatment, x-ray and surgery are available. Another option is to choose no diagnostic studies and/or treatment. Your physician will be happy to discuss these options with you.
If you have any questions, please contact your physician and your doctor will be happy to answer any questions that you may have.